Health
Internal Medicine vs Family Practice – Understanding the Difference
1. Introduction
Understanding the distinctions between internal medicine and family practice is essential when choosing a primary care physician. Both fields offer comprehensive healthcare services, but they differ in focus and scope of practice.
2. Internal Medicine: Focus and Expertise
Internal medicine physicians, also known as internists, specialize in adult healthcare. They are trained to diagnose and manage complex medical conditions affecting various organ systems.
3. Family Practice: Comprehensive Care
Family practice physicians provide primary care to patients of all ages, from infants to seniors. They are skilled in managing a wide range of medical conditions and coordinating care for the entire family.
4. Training and Education
Internal medicine doctors undergo rigorous training in adult medicine during their residency. Family practice physicians receive training in multiple medical specialties, including pediatrics, obstetrics, and gynecology, in addition to adult medicine.
5. Age Group Focus
Internists primarily focus on adult patients, offering specialized care tailored to the unique health needs of adults. Family practice physicians, on the other hand, provide care to patients of all ages, making them a one-stop healthcare provider for families.
6. Disease Management
Internists often manage chronic and complex medical conditions such as diabetes, hypertension, and heart disease. Family practice physicians provide preventive care, acute illness management, and routine screenings for various age groups.
7. Continuity of Care
Internists foster long-term relationships with their adult patients, providing continuity of care across different healthcare settings. Family practice physicians offer continuity of care to individuals and families, addressing their evolving health needs over time.
8. Specialized Referrals
Internists may refer patients to specialists for complex medical conditions or procedures beyond their scope of practice. Family practice physicians coordinate referrals to specialists across different medical disciplines as needed.
9. Preventive Healthcare
Both internal medicine and family practice emphasize preventive healthcare measures such as vaccinations, health screenings, and lifestyle counseling. They play a crucial role in promoting wellness and disease prevention.
10. Primary Care Role
Internists serve as primary care physicians for adults, managing their overall health and coordinating care with other healthcare providers. Family practice physicians serve as primary care providers for individuals and families, offering comprehensive healthcare services.
11. Multidisciplinary Collaboration
Internists collaborate with specialists from various medical disciplines to provide comprehensive care for adult patients. Family practice physicians coordinate care with specialists across different age groups and medical specialties.
12. Patient Population
Internists typically care for a diverse patient population, including young adults, middle-aged individuals, and seniors. Family practice physicians care for patients of all ages, from newborns to elderly individuals, addressing their healthcare needs at every stage of life.
13. Diagnostic Skills
Internists possess advanced diagnostic skills to identify and manage complex medical conditions in adults. Family practice physicians have broad diagnostic skills across different age groups and medical conditions, allowing them to address a wide range of healthcare needs.
14. Chronic Disease Management
Internists specialize in managing chronic diseases prevalent in adults, such as diabetes, cardiovascular disease, and respiratory disorders. Family practice physicians manage chronic diseases across different age groups and provide ongoing support for disease management.
15. Acute Care Expertise
Internists are skilled in managing acute medical conditions and emergencies in adults, ensuring timely diagnosis and treatment. Family practice physicians provide acute care for individuals of all ages, addressing common illnesses and injuries encountered in primary care settings.
16. Patient-Centered Care
Internists and family practice physicians both prioritize patient-centered care, focusing on individual patient needs, preferences, and values. They engage patients in shared decision-making and empower them to take an active role in their healthcare journey.
17. Continual Learning and Development
Internists and family practice physicians engage in ongoing professional development to stay updated with the latest medical advancements and best practices in primary care. They participate in continuing medical education activities to enhance their clinical skills and knowledge.
18. Community Outreach and Education
Internists and family practice physicians play an essential role in community outreach and health education initiatives. They raise awareness about preventive healthcare measures, promote healthy lifestyle choices, and advocate for public health initiatives.
19. Telemedicine Services
Internists and family practice physicians offer telemedicine services to enhance access to healthcare, particularly in remote or underserved areas. Telemedicine allows patients to consult with their primary care providers remotely, improving convenience and accessibility to healthcare services.
20. Importance of Primary Care
Both internal medicine and family practice are integral components of primary care, serving as the first point of contact for patients seeking healthcare services. Primary care providers play a vital role in disease prevention, health promotion, and early intervention, contributing to better health outcomes and reduced healthcare costs.
21. Collaborative Approach
Internists and family practice physicians collaborate with other healthcare professionals, including specialists, nurses, pharmacists, and allied health professionals, to deliver comprehensive and coordinated care to patients. This collaborative approach ensures that patients receive holistic care that addresses their physical, emotional, and social needs.
22. Patient Advocacy
Internists and family practice physicians serve as advocates for their patients, ensuring that their healthcare needs are met and their voices are heard in the healthcare system. They prioritize patient safety, well-being, and satisfaction, striving to provide compassionate and high-quality care to every individual they serve.
23. Research and Innovation
Internists and family practice physicians contribute to medical research and innovation through clinical studies, quality improvement initiatives, and evidence-based practice guidelines. Their research efforts aim to advance medical knowledge, improve patient outcomes, and enhance the delivery of primary care services.
24. Patient-Centered Medical Home
Internists and family practice physicians embrace the patient-centered medical home model, which emphasizes comprehensive, coordinated, and accessible primary care. This model fosters strong patient-provider relationships, promotes care continuity, and enhances healthcare quality and efficiency.
25. Conclusion: Choosing the Right Provider
Whether seeking care from an internist or a family practice physician, patients should prioritize finding a provider who aligns with their healthcare needs, values, and preferences. Both internal medicine and family practice offer high-quality primary care services, ensuring that patients receive personalized, comprehensive, and compassionate healthcare that addresses their unique needs and promotes optimal health and well-being.
Health
Understanding Varicose Veins: Causes and Symptoms
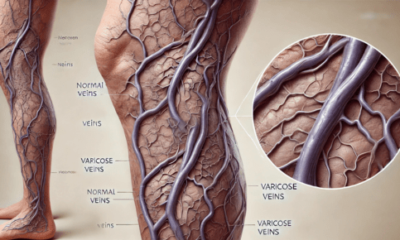
Varicose veins are a common condition that affects millions of people worldwide. These enlarged, twisted veins often appear dark blue or purple and are most commonly found in the legs. While they may seem like a cosmetic issue, varicose veins can lead to more serious health concerns if left untreated. Understanding the causes and symptoms of varicose veins is essential for recognizing this condition early and seeking appropriate treatment.
What Are Varicose Veins?
Varicose veins occur when veins become enlarged and overfilled with blood. This condition typically arises from weakened valves within the veins that are responsible for ensuring blood flows in one direction, toward the heart. When these valves fail, blood can pool in the veins, leading to the characteristic bulging appearance.
Causes of Varicose Veins
Several factors contribute to the development of varicose veins, including:
1. Genetics
A family history of varicose veins can increase your likelihood of developing the condition. If your parents or siblings have had varicose veins, you may be at a higher risk due to inherited weaknesses in the vein walls.
2. Age
As we age, our veins can lose elasticity, making it more difficult for them to effectively push blood back to the heart. This natural aging process can lead to the development of varicose veins.
3. Hormonal Changes
Hormonal fluctuations, particularly in women, can play a significant role in the development of varicose veins. Pregnancy, menstruation, and menopause can increase the risk due to changes in hormone levels that affect vein elasticity and blood flow.
4. Prolonged Standing or Sitting
Occupational factors that require long periods of standing or sitting can contribute to the development of varicose veins. In these positions, blood can pool in the legs, leading to increased pressure on the veins and subsequent enlargement.
5. Obesity
Excess weight places additional pressure on the veins in the lower body. This added strain can weaken the vein walls and valves, increasing the likelihood of developing varicose veins.
6. Injury
Previous injuries to the legs can also lead to varicose veins. Damage to the veins can disrupt blood flow and lead to valve malfunction.
Symptoms of Varicose Veins
While some individuals with varicose veins may not experience noticeable symptoms, others may encounter a range of issues, including:
1. Visible Veins
The most apparent symptom of varicose veins is the presence of swollen, twisted veins that are visible just under the skin’s surface, primarily in the legs.
2. Aching or Heaviness
Many people report feeling a sense of aching or heaviness in their legs, particularly after prolonged periods of standing or sitting. This discomfort can be exacerbated by physical activity.
3. Swelling
Swelling in the legs or ankles is a common symptom associated with varicose veins. This can be particularly noticeable at the end of the day or after extended periods of inactivity.
4. Cramping or Throbbing
Some individuals may experience muscle cramps or throbbing sensations in their legs, especially during the night.
5. Skin Changes
Varicose veins can lead to skin changes in the affected areas. You might notice discoloration, dryness, or even the development of ulcers near the ankles in severe cases.
6. Itching or Burning Sensation
A feeling of itching or burning around the affected veins can also occur, making the condition uncomfortable.
When to Seek Medical Help
If you notice any of the symptoms mentioned above, it’s crucial to consult a healthcare professional. While varicose veins are often considered a cosmetic issue, they can lead to complications such as chronic venous insufficiency, blood clots, or skin ulcers.
Understanding the causes and symptoms of varicose veins is the first step toward effective management and treatment. If you or someone you know is experiencing symptoms associated with varicose veins, it’s essential to seek medical advice promptly. Early intervention can help prevent the progression of the condition and lead to better health outcomes. At Varix Clinic, we specialize in diagnosing and treating varicose veins, offering a range of options tailored to your individual needs. Don’t let varicose veins disrupt your life—reach out to us today for a consultation! Learn more about vascular surgery.
Health
The Role of Medical Coders in Healthcare Compliance

One important component for a hassle-free run in the medical process that is followed in this sector is medical coding.The medical coders in healthcare compliance serve as the liaison between medical services providers, insurance companies and patients. Interpreting patient records, loads of procedures and diagnoses into codes, they see to it that the healthcare facilities do not break any rules.
What is Medical Coding?
In simple words we can say that it’s a description of diagnoses and procedures and converting them into codes. These codes are based on universal coding systems including the International Classification of Diseases (ICD), Current Procedural Terminology (CPT), and Healthcare Common Procedure Coding System. The nature of coding dictates that even a tiny mistake can cause an error to be billed out incorrectly, end up as insurance claim denials and in worst-case scenario, legal actions.
Coverage and Billing Accuracy
Medical coders serve as a critical part of the team that ensures healthcare providers are reimbursed for their services. Every service that is provided to the patient right from a regular checkup to any complicated surgery needs documentation and coding accurately in every possible way. Because even a single mistake in the coding can result in inappropriate billing, which means trouble getting paid on time or outright not being reimbursed. Medical coders ensure accuracy in coding and help hospitals to be reimbursed accordingly & on time, which means seamless financial operations.
Preventing Fraud and Abuse
One of the healthcare industry’s biggest hurdles is preventing fraudulent billing practices. This might mean something like overbilling, billing for services not actually provided or upcoding. Medical coders manage this risk by adhering to very rigid coding standards and guidelines. Because coding regulations are everything to a coder, this ensures that only the legitimate claims (and combinations of conditions) get coded – all preventing potential healthcare fraud and abuse.
Staying Current with the Industry
New treatments, technologies and regulations arise constantly in the healthcare industry. Thus, there are constant changes in the rules and regulations. Medical coders need to be updated with these code changes. Otherwise, they will use old codes that lead to rejection which is an expense to healthcare system. For example, changes in the ICD codes or updates to CMS policies can drastically change how medical procedures are coded and billed. Medical coders must continually learn and adapt to be able to do their jobs correctly and ensure that healthcare facilities stay compliant with the ever-changing coding regulations.
Wrapping Up
Technology has come a long way, and this means that the field of medical coding is richer for it. Nowadays, automated coding systems and artificial intelligence tools are introduced to help medical coders spot the right codes quickly. But humans are still needed to verify whether automated systems are accurate and process cases that require human understanding. Skilled coders using the technology push compliance, accuracy, and efficiency in coding.
Health
Beyond the Spa: Unpacking the Transformative Power of the Hoffman Process

In the realm of wellness, health retreats have become increasingly popular, offering a tranquil escape from the stresses of modern life. However, for those seeking more than just a fleeting respite, the Hoffman Process presents a unique and profound opportunity for emotional healing. This intensive program transcends the traditional boundaries of a Victorian health retreat, anxiety retreat, or spirit retreat, to delve into the complexities of the human psyche, fostering lasting transformation and mental well-being.
A Holistic Approach to Healing
The Hoffman Process is an 8-day intensive program that combines elements of psychology, spirituality, and personal development to address the root causes of emotional pain. Unlike a traditional health retreat, which may focus primarily on physical wellness, the Hoffman Process recognizes that true healing requires a holistic approach. By integrating techniques from various disciplines, participants are guided on a journey of self-discovery, confronting and releasing negative patterns, emotions, and beliefs that have held them back.
Uncovering the Sources of Suffering
One of the key aspects of the Hoffman Process is its focus on identifying and resolving childhood trauma and negative childhood experiences. Through a series of exercises, lectures, and group sessions, participants gain insight into how these early experiences have shaped their relationships, behaviors, and worldview. This understanding enables them to break free from destructive patterns and develop more compassionate, empowering relationships with themselves and others.
The Role of Emotional Release
Emotional release is a crucial component of the Hoffman Process. By creating a safe and supportive environment, participants are encouraged to confront and express repressed emotions, often linked to past traumas or unresolved conflicts. This cathartic process allows individuals to release the emotional burden they’ve carried, paving the way for renewed energy, clarity, and purpose.
Rebuilding and Renewal
Following the intensive emotional release, the Hoffman Process focuses on rebuilding and renewal. Participants engage in exercises designed to rewire negative thought patterns, cultivate self-awareness, and develop healthy communication skills. This empowering phase of the program enables individuals to reintegrate into their daily lives with increased confidence, resilience, and emotional intelligence.
A Spirit Retreat for the Modern Era
While the Hoffman Process shares some similarities with traditional spirit retreats, its emphasis on emotional healing and personal growth sets it apart. The program’s holistic approach acknowledges the interconnectedness of body, mind, and spirit, providing a comprehensive framework for transformation. By addressing the complexities of the human experience, the Hoffman Process offers a profoundly spiritual experience that extends far beyond the retreat itself.
A Mental Health Retreat with Lasting Impact
The Hoffman Process is not merely a mental health retreat; it’s a transformative journey that equips participants with the tools and insights necessary for sustained growth. By confronting and overcoming deep-seated emotional challenges, individuals can experience profound shifts in their relationships, career, and overall well-being. The program’s long-term impact is a testament to its effectiveness in fostering genuine, lasting change.
Conclusion
For those seeking more than just a temporary escape, the Hoffman Process offers a life-changing opportunity for emotional healing and transformation. By moving beyond the confines of a traditional health retreat, anxiety retreat, or spirit retreat, this intensive program addresses the complexities of the human experience, empowering individuals to reclaim their emotional well-being and live a more authentic, fulfilling life. If you’re ready to embark on a profound journey of self-discovery and healing, the Hoffman Process may be the catalyst for the transformative change you’ve been seeking.
-

 Dental4 days ago
Dental4 days agoWhat Are The Factors That Directly Affect The Healing of Dental Implants?
-

 Health1 day ago
Health1 day agoThe Role of Medical Coders in Healthcare Compliance
-

 Dental1 day ago
Dental1 day agoWhat to Expect From Berwick Dentists at Berwick Dental Centre
-
 Health1 day ago
Health1 day agoUnderstanding Varicose Veins: Causes and Symptoms
