Health
Exploring Genetic Disorders – Differentiating Between Genetic and Non-Genetic Conditions
Genetic disorders arise from abnormalities in an individual’s DNA, leading to various health conditions. However, not all medical conditions are genetic in nature. Let’s identify which of the following conditions is not a genetic disorder.
1. Genetic Disorders Defined
Genetic disorders result from mutations or changes in genes, chromosomes, or the overall structure of DNA. These alterations can affect an individual’s physical characteristics, development, and overall health.
2. Inherited Genetic Disorders
Some genetic disorders are inherited from one or both parents and can be passed down through generations. Examples include cystic fibrosis, Huntington’s disease, and sickle cell anemia.
3. Non-Inherited Genetic Disorders
Non-inherited genetic disorders, also known as spontaneous mutations, occur randomly during the formation of reproductive cells or early stages of embryonic development. Examples include Down syndrome and Edwards syndrome.
4. Environmental Factors
Some medical conditions are not caused by genetic factors but rather by environmental factors such as exposure to toxins, infections, or injuries. Examples include lung cancer from smoking and lead poisoning from environmental exposure.
5. Infectious Diseases
Infectious diseases are caused by pathogens such as bacteria, viruses, fungi, or parasites and are not considered genetic disorders. Examples include influenza, tuberculosis, and malaria.
6. Nutritional Deficiencies
Medical conditions resulting from inadequate intake or absorption of essential nutrients are not genetic disorders. Examples include scurvy due to vitamin C deficiency and rickets due to vitamin D deficiency.
7. Hormonal Imbalances
Hormonal imbalances, whether due to endocrine disorders or other factors, are not genetic disorders but rather disruptions in the body’s hormonal regulation system. Examples include diabetes mellitus and thyroid disorders.
8. Autoimmune Diseases
Autoimmune diseases occur when the immune system mistakenly attacks the body’s own tissues, leading to inflammation and tissue damage. These conditions are not genetic disorders but rather dysregulations of the immune system. Examples include rheumatoid arthritis and lupus.
9. Mental Health Disorders
Mental health disorders, such as depression, anxiety disorders, and schizophrenia, have complex etiologies involving genetic, environmental, and psychological factors. While genetics may play a role, these conditions are not solely genetic disorders.
10. Traumatic Injuries
Injuries resulting from accidents, falls, or trauma are not genetic disorders but rather acute or chronic physical damage to tissues or organs. Examples include fractures, concussions, and spinal cord injuries.
11. Developmental Disorders
Developmental disorders, such as autism spectrum disorder and attention-deficit/hyperactivity disorder (ADHD), have multifactorial origins involving genetic, environmental, and developmental factors. They are not exclusively genetic disorders.
12. Congenital Anomalies
Congenital anomalies, also known as birth defects, can result from genetic, environmental, or unknown causes. Examples include cleft lip and palate, congenital heart defects, and neural tube defects.
13. Degenerative Diseases
Degenerative diseases, such as Alzheimer’s disease and Parkinson’s disease, are characterized by progressive deterioration of specific tissues or organs over time. While genetics may contribute to susceptibility, they are not strictly genetic disorders.
14. Lifestyle-Related Conditions
Medical conditions influenced by lifestyle choices, such as obesity, hypertension, and type 2 diabetes, are not genetic disorders but rather result from diet, physical activity, and other lifestyle factors.
15. Infectious Diseases
Infectious diseases, such as the common cold, flu, and gastroenteritis, are caused by pathogens such as viruses, bacteria, fungi, or parasites and are not considered genetic disorders.
16. Environmental Toxins
Exposure to environmental toxins, pollutants, or chemicals can lead to health conditions such as lead poisoning, mercury poisoning, and pesticide exposure-related illnesses. These are not genetic disorders.
17. Physical Trauma
Injuries resulting from accidents, falls, or physical trauma, such as fractures, sprains, and lacerations, are not genetic disorders but rather acute injuries to the body’s tissues.
18. Lifestyle Factors
Medical conditions influenced by lifestyle choices, such as smoking-related lung cancer, alcohol-related liver disease, and sedentary lifestyle-related obesity, are not genetic disorders.
19. Aging-Related Conditions
Age-related conditions, such as osteoarthritis, osteoporosis, and age-related macular degeneration, are not genetic disorders but rather result from the natural aging process and environmental factors.
20. Inflammatory Conditions
Inflammatory conditions, such as asthma, inflammatory bowel disease (IBD), and psoriasis, are not genetic disorders but rather result from dysregulation of the immune system and environmental triggers.
21. Endocrine Disorders
Endocrine disorders, such as diabetes mellitus and thyroid disorders, are not genetic disorders but rather result from dysregulation of hormone production or action in the body.
22. Infectious Diseases
Infectious diseases, such as the flu, tuberculosis, and HIV/AIDS, are caused by pathogens such as viruses, bacteria, fungi, or parasites and are not considered genetic disorders.
23. Lifestyle-Related Conditions
Medical conditions influenced by lifestyle choices, such as obesity, hypertension, and type 2 diabetes, are not genetic disorders but rather result from diet, physical activity, and other lifestyle factors.
24. Environmental Toxins
Exposure to environmental toxins, pollutants, or chemicals can lead to health conditions such as lead poisoning, mercury poisoning, and pesticide exposure-related illnesses. These are not genetic disorders.
25. Physical Trauma
Injuries resulting from accidents, falls, or physical trauma, such as fractures, sprains, and lacerations, are not genetic disorders but rather acute injuries to the body’s tissues.
Health
Orthopedic Surgeons And Their Crucial Role In Treating Athletic Injuries

Athletic injuries can sideline even the most dedicated athletes. Orthopedic surgeons play a crucial role in getting them back on track. They diagnose, treat, and help prevent injuries related to sports and physical activities. With specialized training, these experts understand the intricate details of bones, joints, and muscles. Places like Sports Medicine Associates of San Antonio bring together skilled orthopedic surgeons to provide comprehensive care. Teams rely on these professionals to ensure athletes recover stronger and faster.
Understanding the Role of Orthopedic Surgeons
Orthopedic surgeons focus on the musculoskeletal system. This includes bones, joints, ligaments, tendons, and muscles. When athletes get hurt, these surgeons identify the problem and offer solutions. Their training allows them to perform surgeries that repair or replace damaged parts of the body. They also use non-surgical methods like physical therapy.
For those interested in learning more about the field, the Association of American Medical Colleges offers detailed insights into what orthopedic surgery entails.
Common Athletic Injuries Treated by Orthopedic Surgeons
Orthopedic surgeons deal with a range of sports-related injuries. Below are some common ones:
- Knee Injuries: Torn ligaments like the ACL are frequent in sports.
- Shoulder Injuries: Rotator cuff tears affect many athletes.
- Ankle Sprains: These occur often during running or jumping activities.
These injuries can vary in severity. Orthopedic surgeons assess and decide the best course of action. This can range from rest and rehabilitation to surgery.
Comparison of Treatment Options
| Injury | Non-Surgical Treatment | Surgical Treatment |
| Knee Injury | Physical therapy, Bracing | ACL Reconstruction |
| Shoulder Injury | Rest, Strengthening exercises | Rotator Cuff Repair |
| Ankle Sprain | R.I.C.E (Rest, Ice, Compression, Elevation) | Ankle Ligament Reconstruction |
The Importance of Early Intervention
Acting quickly is vital in sports injuries. Early intervention can prevent further complications and expedite recovery. Orthopedic surgeons work with athletes to create a personalized plan. This ensures that recovery is both effective and swift.
As highlighted by the Centers for Disease Control and Prevention (CDC), understanding the nature of the injury and responding promptly can drastically improve outcomes.
Prevention and Education
Beyond treatment, orthopedic surgeons focus on prevention. They educate athletes on proper techniques and warm-up routines. This knowledge helps reduce the risk of future injuries. Wearing appropriate gear and maintaining fitness levels are also key aspects of prevention.
Incorporating these strategies can help athletes continue to enjoy their sports while minimizing injury risks.
Conclusion
Orthopedic surgeons are essential in the realm of sports medicine. Their expertise ensures athletes receive the best care. From diagnosing issues to offering treatment and preventive advice, they cover all bases. With their guidance, athletes can focus on what they love—playing and excelling in their chosen sports.
Health
Understanding Varicose Veins: Causes and Symptoms
Varicose veins are a common condition that affects millions of people worldwide. These enlarged, twisted veins often appear dark blue or purple and are most commonly found in the legs. While they may seem like a cosmetic issue, varicose veins can lead to more serious health concerns if left untreated. Understanding the causes and symptoms of varicose veins is essential for recognizing this condition early and seeking appropriate treatment.
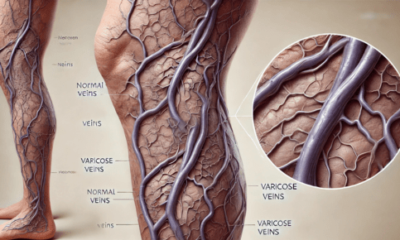
What Are Varicose Veins?
Varicose veins occur when veins become enlarged and overfilled with blood. This condition typically arises from weakened valves within the veins that are responsible for ensuring blood flows in one direction, toward the heart. When these valves fail, blood can pool in the veins, leading to the characteristic bulging appearance.
Causes of Varicose Veins
Several factors contribute to the development of varicose veins, including:
1. Genetics
A family history of varicose veins can increase your likelihood of developing the condition. If your parents or siblings have had varicose veins, you may be at a higher risk due to inherited weaknesses in the vein walls.
2. Age
As we age, our veins can lose elasticity, making it more difficult for them to effectively push blood back to the heart. This natural aging process can lead to the development of varicose veins.
3. Hormonal Changes
Hormonal fluctuations, particularly in women, can play a significant role in the development of varicose veins. Pregnancy, menstruation, and menopause can increase the risk due to changes in hormone levels that affect vein elasticity and blood flow.
4. Prolonged Standing or Sitting
Occupational factors that require long periods of standing or sitting can contribute to the development of varicose veins. In these positions, blood can pool in the legs, leading to increased pressure on the veins and subsequent enlargement.
5. Obesity
Excess weight places additional pressure on the veins in the lower body. This added strain can weaken the vein walls and valves, increasing the likelihood of developing varicose veins.
6. Injury
Previous injuries to the legs can also lead to varicose veins. Damage to the veins can disrupt blood flow and lead to valve malfunction.
Symptoms of Varicose Veins
While some individuals with varicose veins may not experience noticeable symptoms, others may encounter a range of issues, including:
1. Visible Veins
The most apparent symptom of varicose veins is the presence of swollen, twisted veins that are visible just under the skin’s surface, primarily in the legs.
2. Aching or Heaviness
Many people report feeling a sense of aching or heaviness in their legs, particularly after prolonged periods of standing or sitting. This discomfort can be exacerbated by physical activity.
3. Swelling
Swelling in the legs or ankles is a common symptom associated with varicose veins. This can be particularly noticeable at the end of the day or after extended periods of inactivity.
4. Cramping or Throbbing
Some individuals may experience muscle cramps or throbbing sensations in their legs, especially during the night.
5. Skin Changes
Varicose veins can lead to skin changes in the affected areas. You might notice discoloration, dryness, or even the development of ulcers near the ankles in severe cases.
6. Itching or Burning Sensation
A feeling of itching or burning around the affected veins can also occur, making the condition uncomfortable.
When to Seek Medical Help
If you notice any of the symptoms mentioned above, it’s crucial to consult a healthcare professional. While varicose veins are often considered a cosmetic issue, they can lead to complications such as chronic venous insufficiency, blood clots, or skin ulcers.
Understanding the causes and symptoms of varicose veins is the first step toward effective management and treatment. If you or someone you know is experiencing symptoms associated with varicose veins, it’s essential to seek medical advice promptly. Early intervention can help prevent the progression of the condition and lead to better health outcomes. At Varix Clinic, we specialize in diagnosing and treating varicose veins, offering a range of options tailored to your individual needs. Don’t let varicose veins disrupt your life—reach out to us today for a consultation! Learn more about vascular surgery.
Health
The Role of Medical Coders in Healthcare Compliance

One important component for a hassle-free run in the medical process that is followed in this sector is medical coding.The medical coders in healthcare compliance serve as the liaison between medical services providers, insurance companies and patients. Interpreting patient records, loads of procedures and diagnoses into codes, they see to it that the healthcare facilities do not break any rules.
What is Medical Coding?
In simple words we can say that it’s a description of diagnoses and procedures and converting them into codes. These codes are based on universal coding systems including the International Classification of Diseases (ICD), Current Procedural Terminology (CPT), and Healthcare Common Procedure Coding System. The nature of coding dictates that even a tiny mistake can cause an error to be billed out incorrectly, end up as insurance claim denials and in worst-case scenario, legal actions.
Coverage and Billing Accuracy
Medical coders serve as a critical part of the team that ensures healthcare providers are reimbursed for their services. Every service that is provided to the patient right from a regular checkup to any complicated surgery needs documentation and coding accurately in every possible way. Because even a single mistake in the coding can result in inappropriate billing, which means trouble getting paid on time or outright not being reimbursed. Medical coders ensure accuracy in coding and help hospitals to be reimbursed accordingly & on time, which means seamless financial operations.
Preventing Fraud and Abuse
One of the healthcare industry’s biggest hurdles is preventing fraudulent billing practices. This might mean something like overbilling, billing for services not actually provided or upcoding. Medical coders manage this risk by adhering to very rigid coding standards and guidelines. Because coding regulations are everything to a coder, this ensures that only the legitimate claims (and combinations of conditions) get coded – all preventing potential healthcare fraud and abuse.
Staying Current with the Industry
New treatments, technologies and regulations arise constantly in the healthcare industry. Thus, there are constant changes in the rules and regulations. Medical coders need to be updated with these code changes. Otherwise, they will use old codes that lead to rejection which is an expense to healthcare system. For example, changes in the ICD codes or updates to CMS policies can drastically change how medical procedures are coded and billed. Medical coders must continually learn and adapt to be able to do their jobs correctly and ensure that healthcare facilities stay compliant with the ever-changing coding regulations.
Wrapping Up
Technology has come a long way, and this means that the field of medical coding is richer for it. Nowadays, automated coding systems and artificial intelligence tools are introduced to help medical coders spot the right codes quickly. But humans are still needed to verify whether automated systems are accurate and process cases that require human understanding. Skilled coders using the technology push compliance, accuracy, and efficiency in coding.
-

 Health2 days ago
Health2 days agoThe Role of Medical Coders in Healthcare Compliance
-

 Dental2 days ago
Dental2 days agoWhat to Expect From Berwick Dentists at Berwick Dental Centre
-
 Health2 days ago
Health2 days agoUnderstanding Varicose Veins: Causes and Symptoms
-

 Health13 hours ago
Health13 hours agoOrthopedic Surgeons And Their Crucial Role In Treating Athletic Injuries
-

 Dental12 hours ago
Dental12 hours agoHow A General Dentist Treats Dental Trauma
-
 Treatments12 hours ago
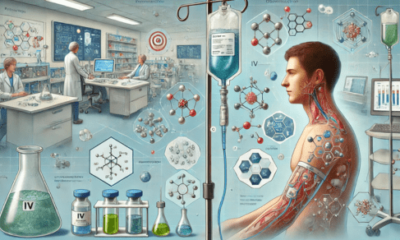
Treatments12 hours agoIn Depth: The Pharmacology Of IV Medications
-
 Treatments12 hours ago
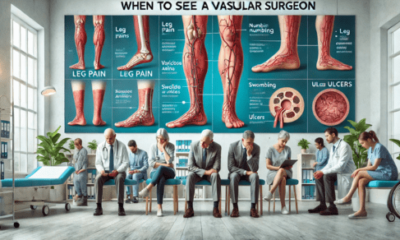
Treatments12 hours agoWhen To See A Vascular Surgeon: Understanding The Signs And Symptoms
