Health
Understanding Bone Profile Blood Tests – What Diseases Can They Detect
1. Introduction
Bone profile blood tests are valuable diagnostic tools used to assess bone health and detect various diseases affecting the skeletal system.
2. Bone Health Evaluation
These tests provide valuable information about bone mineral density, calcium levels, and other markers related to bone metabolism.
3. Osteoporosis
Bone profile blood tests can indicate the presence of osteoporosis, a condition characterized by weakened bones and increased risk of fractures.
4. Osteopenia
Osteopenia, a precursor to osteoporosis, can also be detected through abnormalities in bone profile blood test results.
5. Calcium Imbalance
Abnormal levels of calcium in the blood, either too high (hypercalcemia) or too low (hypocalcemia), can indicate underlying health issues affecting the bones.
6. Vitamin D Deficiency
Bone profile blood tests may reveal low levels of vitamin D, which can contribute to bone weakening and disorders like osteomalacia.
7. Parathyroid Disorders
Disorders of the parathyroid glands, such as hyperparathyroidism or hypoparathyroidism, can affect calcium regulation and bone health, detectable through bone profile tests.
8. Paget’s Disease
Paget’s disease of the bone, characterized by abnormal bone remodeling, can be detected through specific markers in bone profile blood tests.
9. Bone Cancer
Certain bone cancers, such as osteosarcoma or multiple myeloma, can alter bone metabolism, leading to abnormalities in bone profile test results.
10. Metabolic Bone Diseases
Metabolic bone diseases like hyperthyroidism or hypothyroidism can impact bone health and may be reflected in bone profile blood test results.
11. Renal Osteodystrophy
Kidney disease can affect calcium and phosphate levels in the blood, leading to bone abnormalities detectable through bone profile testing.
12. Rheumatoid Arthritis
Rheumatoid arthritis and other autoimmune disorders can cause inflammation and damage to the joints and bones, which may be reflected in bone profile test results.
13. Malabsorption Syndromes
Conditions that affect nutrient absorption in the gastrointestinal tract, such as celiac disease or inflammatory bowel disease, can impact bone health and show abnormalities in bone profile tests.
14. Hormonal Imbalances
Hormonal imbalances, including thyroid disorders or adrenal gland disorders, can influence bone metabolism and may be detected through bone profile blood tests.
15. Monitoring Treatment Response
Bone profile blood tests are also used to monitor the effectiveness of treatments for bone-related conditions, such as osteoporosis medications or vitamin D supplementation.
16. Fracture Risk Assessment
Bone profile tests can help assess an individual’s risk of fractures by evaluating bone density and other markers of bone health.
17. Comprehensive Evaluation
Bone profile blood tests provide a comprehensive evaluation of bone health, aiding in the diagnosis and management of various bone-related diseases and conditions.
18. Preventive Screening
Early detection of bone abnormalities through bone profile testing allows for timely intervention and preventive measures to minimize the risk of fractures and other complications.
19. Consultation with Healthcare Provider
Interpreting bone profile blood test results requires consultation with a healthcare provider, who can provide personalized recommendations based on individual health status and risk factors.
20. Lifestyle Modifications
In addition to medical interventions, lifestyle modifications such as dietary changes, weight-bearing exercises, and smoking cessation can help improve bone health and prevent bone-related diseases.
21. Collaboration with Specialists
Managing bone-related diseases often involves collaboration with specialists such as endocrinologists, rheumatologists, or orthopedic surgeons for comprehensive care.
22. Patient Education
Patient education plays a crucial role in promoting bone health awareness and empowering individuals to take proactive steps in managing bone-related diseases.
23. Regular Monitoring
Regular monitoring of bone profile parameters allows for ongoing assessment of bone health and adjustment of treatment plans as needed.
24. Conclusion
In conclusion, bone profile blood tests serve as valuable diagnostic tools for detecting a wide range of diseases and conditions affecting bone health. Early detection and intervention are essential for minimizing the impact of these conditions and promoting overall well-being.
25. Resources
For more information about bone profile blood tests and bone-related diseases, consult with a healthcare provider or refer to reputable medical resources and organizations specializing in bone health.
Health
Orthopedic Surgeons And Their Crucial Role In Treating Athletic Injuries

Athletic injuries can sideline even the most dedicated athletes. Orthopedic surgeons play a crucial role in getting them back on track. They diagnose, treat, and help prevent injuries related to sports and physical activities. With specialized training, these experts understand the intricate details of bones, joints, and muscles. Places like Sports Medicine Associates of San Antonio bring together skilled orthopedic surgeons to provide comprehensive care. Teams rely on these professionals to ensure athletes recover stronger and faster.
Understanding the Role of Orthopedic Surgeons
Orthopedic surgeons focus on the musculoskeletal system. This includes bones, joints, ligaments, tendons, and muscles. When athletes get hurt, these surgeons identify the problem and offer solutions. Their training allows them to perform surgeries that repair or replace damaged parts of the body. They also use non-surgical methods like physical therapy.
For those interested in learning more about the field, the Association of American Medical Colleges offers detailed insights into what orthopedic surgery entails.
Common Athletic Injuries Treated by Orthopedic Surgeons
Orthopedic surgeons deal with a range of sports-related injuries. Below are some common ones:
- Knee Injuries: Torn ligaments like the ACL are frequent in sports.
- Shoulder Injuries: Rotator cuff tears affect many athletes.
- Ankle Sprains: These occur often during running or jumping activities.
These injuries can vary in severity. Orthopedic surgeons assess and decide the best course of action. This can range from rest and rehabilitation to surgery.
Comparison of Treatment Options
| Injury | Non-Surgical Treatment | Surgical Treatment |
| Knee Injury | Physical therapy, Bracing | ACL Reconstruction |
| Shoulder Injury | Rest, Strengthening exercises | Rotator Cuff Repair |
| Ankle Sprain | R.I.C.E (Rest, Ice, Compression, Elevation) | Ankle Ligament Reconstruction |
The Importance of Early Intervention
Acting quickly is vital in sports injuries. Early intervention can prevent further complications and expedite recovery. Orthopedic surgeons work with athletes to create a personalized plan. This ensures that recovery is both effective and swift.
As highlighted by the Centers for Disease Control and Prevention (CDC), understanding the nature of the injury and responding promptly can drastically improve outcomes.
Prevention and Education
Beyond treatment, orthopedic surgeons focus on prevention. They educate athletes on proper techniques and warm-up routines. This knowledge helps reduce the risk of future injuries. Wearing appropriate gear and maintaining fitness levels are also key aspects of prevention.
Incorporating these strategies can help athletes continue to enjoy their sports while minimizing injury risks.
Conclusion
Orthopedic surgeons are essential in the realm of sports medicine. Their expertise ensures athletes receive the best care. From diagnosing issues to offering treatment and preventive advice, they cover all bases. With their guidance, athletes can focus on what they love—playing and excelling in their chosen sports.
Health
Understanding Varicose Veins: Causes and Symptoms
Varicose veins are a common condition that affects millions of people worldwide. These enlarged, twisted veins often appear dark blue or purple and are most commonly found in the legs. While they may seem like a cosmetic issue, varicose veins can lead to more serious health concerns if left untreated. Understanding the causes and symptoms of varicose veins is essential for recognizing this condition early and seeking appropriate treatment.
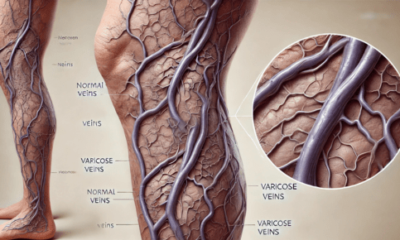
What Are Varicose Veins?
Varicose veins occur when veins become enlarged and overfilled with blood. This condition typically arises from weakened valves within the veins that are responsible for ensuring blood flows in one direction, toward the heart. When these valves fail, blood can pool in the veins, leading to the characteristic bulging appearance.
Causes of Varicose Veins
Several factors contribute to the development of varicose veins, including:
1. Genetics
A family history of varicose veins can increase your likelihood of developing the condition. If your parents or siblings have had varicose veins, you may be at a higher risk due to inherited weaknesses in the vein walls.
2. Age
As we age, our veins can lose elasticity, making it more difficult for them to effectively push blood back to the heart. This natural aging process can lead to the development of varicose veins.
3. Hormonal Changes
Hormonal fluctuations, particularly in women, can play a significant role in the development of varicose veins. Pregnancy, menstruation, and menopause can increase the risk due to changes in hormone levels that affect vein elasticity and blood flow.
4. Prolonged Standing or Sitting
Occupational factors that require long periods of standing or sitting can contribute to the development of varicose veins. In these positions, blood can pool in the legs, leading to increased pressure on the veins and subsequent enlargement.
5. Obesity
Excess weight places additional pressure on the veins in the lower body. This added strain can weaken the vein walls and valves, increasing the likelihood of developing varicose veins.
6. Injury
Previous injuries to the legs can also lead to varicose veins. Damage to the veins can disrupt blood flow and lead to valve malfunction.
Symptoms of Varicose Veins
While some individuals with varicose veins may not experience noticeable symptoms, others may encounter a range of issues, including:
1. Visible Veins
The most apparent symptom of varicose veins is the presence of swollen, twisted veins that are visible just under the skin’s surface, primarily in the legs.
2. Aching or Heaviness
Many people report feeling a sense of aching or heaviness in their legs, particularly after prolonged periods of standing or sitting. This discomfort can be exacerbated by physical activity.
3. Swelling
Swelling in the legs or ankles is a common symptom associated with varicose veins. This can be particularly noticeable at the end of the day or after extended periods of inactivity.
4. Cramping or Throbbing
Some individuals may experience muscle cramps or throbbing sensations in their legs, especially during the night.
5. Skin Changes
Varicose veins can lead to skin changes in the affected areas. You might notice discoloration, dryness, or even the development of ulcers near the ankles in severe cases.
6. Itching or Burning Sensation
A feeling of itching or burning around the affected veins can also occur, making the condition uncomfortable.
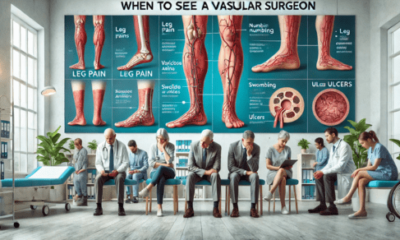
When to Seek Medical Help
If you notice any of the symptoms mentioned above, it’s crucial to consult a healthcare professional. While varicose veins are often considered a cosmetic issue, they can lead to complications such as chronic venous insufficiency, blood clots, or skin ulcers.
Understanding the causes and symptoms of varicose veins is the first step toward effective management and treatment. If you or someone you know is experiencing symptoms associated with varicose veins, it’s essential to seek medical advice promptly. Early intervention can help prevent the progression of the condition and lead to better health outcomes. At Varix Clinic, we specialize in diagnosing and treating varicose veins, offering a range of options tailored to your individual needs. Don’t let varicose veins disrupt your life—reach out to us today for a consultation! Learn more about vascular surgery.
Health
The Role of Medical Coders in Healthcare Compliance

One important component for a hassle-free run in the medical process that is followed in this sector is medical coding.The medical coders in healthcare compliance serve as the liaison between medical services providers, insurance companies and patients. Interpreting patient records, loads of procedures and diagnoses into codes, they see to it that the healthcare facilities do not break any rules.
What is Medical Coding?
In simple words we can say that it’s a description of diagnoses and procedures and converting them into codes. These codes are based on universal coding systems including the International Classification of Diseases (ICD), Current Procedural Terminology (CPT), and Healthcare Common Procedure Coding System. The nature of coding dictates that even a tiny mistake can cause an error to be billed out incorrectly, end up as insurance claim denials and in worst-case scenario, legal actions.
Coverage and Billing Accuracy
Medical coders serve as a critical part of the team that ensures healthcare providers are reimbursed for their services. Every service that is provided to the patient right from a regular checkup to any complicated surgery needs documentation and coding accurately in every possible way. Because even a single mistake in the coding can result in inappropriate billing, which means trouble getting paid on time or outright not being reimbursed. Medical coders ensure accuracy in coding and help hospitals to be reimbursed accordingly & on time, which means seamless financial operations.
Preventing Fraud and Abuse
One of the healthcare industry’s biggest hurdles is preventing fraudulent billing practices. This might mean something like overbilling, billing for services not actually provided or upcoding. Medical coders manage this risk by adhering to very rigid coding standards and guidelines. Because coding regulations are everything to a coder, this ensures that only the legitimate claims (and combinations of conditions) get coded – all preventing potential healthcare fraud and abuse.
Staying Current with the Industry
New treatments, technologies and regulations arise constantly in the healthcare industry. Thus, there are constant changes in the rules and regulations. Medical coders need to be updated with these code changes. Otherwise, they will use old codes that lead to rejection which is an expense to healthcare system. For example, changes in the ICD codes or updates to CMS policies can drastically change how medical procedures are coded and billed. Medical coders must continually learn and adapt to be able to do their jobs correctly and ensure that healthcare facilities stay compliant with the ever-changing coding regulations.
Wrapping Up
Technology has come a long way, and this means that the field of medical coding is richer for it. Nowadays, automated coding systems and artificial intelligence tools are introduced to help medical coders spot the right codes quickly. But humans are still needed to verify whether automated systems are accurate and process cases that require human understanding. Skilled coders using the technology push compliance, accuracy, and efficiency in coding.
-

 Health2 days ago
Health2 days agoThe Role of Medical Coders in Healthcare Compliance
-

 Dental2 days ago
Dental2 days agoWhat to Expect From Berwick Dentists at Berwick Dental Centre
-
 Health2 days ago
Health2 days agoUnderstanding Varicose Veins: Causes and Symptoms
-

 Health7 hours ago
Health7 hours agoOrthopedic Surgeons And Their Crucial Role In Treating Athletic Injuries
-

 Dental7 hours ago
Dental7 hours agoHow A General Dentist Treats Dental Trauma
-
 Treatments7 hours ago
Treatments7 hours agoIn Depth: The Pharmacology Of IV Medications
-
 Treatments7 hours ago
Treatments7 hours agoWhen To See A Vascular Surgeon: Understanding The Signs And Symptoms
